Shingles Part I: Understanding the Viral Phases
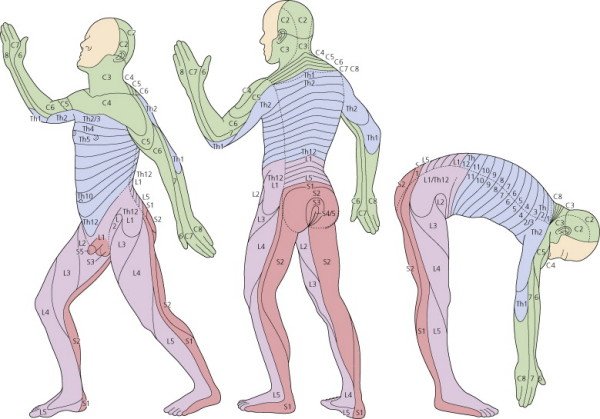
Herpes Zoster (a.k.a. Shingles) is an acute skin infection associated with the reactivation of the varicella-zoster virus (the virus that causes chickenpox). During chicken pox infection, the virus enters the cutaneous nerves and then travels to the dorsal root ganglia where it lies dormant until something triggers it to become active again. Stress, illness, emotional upset, T-cell immuno-suppressant drugs, fatigue and radiation therapy (any circumstances that compromise a patient’s immunity) can trigger the latent virus to travel back down the sensory nerve to infect the surface of the skin (along a single dermatome).
There are 3 distinct clinical phases of shingles: prodromal, active, and chronic.
The skin rash of Herpes Zoster will develop along a single dermatome (although if severe, may affect adjacent dermatomes).
1. PRODROMAL PHASE: Prodromal refers to the initial phase of an illness, the interval between the earliest symptoms and the appearance of a rash. In the case of Herpes Zoster, this phase can last a few days to 3 weeks before a rash actually appears (typically 4 to 5 days). Pain lasting longer than 3 weeks has been reported and this can cause difficulty in differentiating the source of the pain until the characteristic rash erupts (pre-herpetic pain has been mistaken for migraine, pleurisy, abdominal disease or cardiac pain). Recognizing that shingles pain follows the dermatome can help diagnosis in this early stage. Patients and practitioners take note: we can achieve the best clinical results if we begin treatment (such as herbs) during this initial phase.
Skin Symptoms to watch for: (most often on the sides of the torso, on the chest, along the spine, on the lower back, but possibly on the face (usually forehead) or limbs)
Pain (sharp, stabbing, pricking, and/or shooting)
Tenderness
Itching
Burning
Numbness
Tingling
Heightened sensitivity to mild stimuli
Generalized Symptoms to watch for: (flu-like symptoms that tend to resolve when the rash erupts)
Headache
Slight fever
Fatigue
Decreased appetite
Regional lymphadenopathy (swollen lymph nodes)
2. ACTIVE PHASE: Appearance of a rash that manifests as clusters of small red vesicles like beads on an erythematous base (red skin) with burning pain (can be quite severe). The pain is a result of inflammation of the affected nerve, not the lesions themselves. Red patches of blisters (with clear fluid in them) form along the affected nerve pathway (usually only on one side of the body) and form a chain-like distribution of lesions. Occasionally a few vesicles will appear across the midline. Within a few days, blisters become yellow and by the end of the week they start to crust over. New lesions can continue to erupt for the first week. Because the lesions are filled with virus, they can spread easily and are contagious, so patients should avoid touching them. The rash usually resolves within 2 to 3 weeks.
Rash erupts on one side of torso, red base with blisters that look a lot like poison ivy.
3. CHRONIC PHASE: While the skin itself typically heals without scarring, herpes zoster can sometimes become chronic, manifesting as painful patches of skin (“post-herpetic neuralgia”, PHN). Burning, “ice-burning”, stabbing, or shooting pains can last weeks, months, or even years after the rash has resolved. This is because the injured nerve can fire spontaneously, has a lower activation threshold and has an exaggerated response to stimuli. The central nervous system may also develop inappropriate responses to the signals received from the damaged peripheral nerve. Occasionally, vision or hearing impairment may result if the virus affects certain cranial nerves. The latent varicella-zoster virus typically reactivates only once in a person’s lifetime, but it is possible to develop shingles 2 or 3 times in a lifetime. The elderly, immuno-compromised individuals, and patients taking immuno-suppressant drugs are more likely to suffer from PHN. For these patients pain can be severe or even disabling.
OPHTHALMIC ZOSTER: In 10 to 15% of shingles cases, the varicella-zoster virus can become reactivated in the 5th cranial nerve (the trigeminal nerve). The trigeminal nerve has 3 main branches: the ophthalmic, the maxillary, and the mandibular. The ophthalmic branch of the trigeminal nerve divides further into 3 more branches: the frontal, the lacrimal and the nasociliary. If shingles develops along any of these 3 branches it is called herpes zoster ophthalmicus. When the virus affects the nasociliary branch of the ophthalmic nerve, the rash will appear at the side or tip of the nose. This often is an indication that serious ocular complications are possible and treatment must not be delayed to avoid the risk of sight loss.
Ophthalmic Zoster. Shingles lesions at the side of the nose can indicate the most serious ocular complications. (Copyright © 2012 Elsevier Inc.)
SHINGLES TREATMENT: Chinese medicine is a very effective form of treatment in most cases of shingles (alone or in conjunction with western antivirals), especially if started in the prodromal (pre-eruptive) phase. Treatment is aimed at accelerating the healing and preventing post-herpetic pain and additional complications.
Acupuncture can effectively address pain, accelerate the healing of lesions, and reduce nerve inflammation. Chinese herbs also act to heal lesions and reduce nerve inflammation and additionally they have very strong antiviral properties. The sooner treatment is started, the better the results. TCM treatment of shingles and management of PHN will be covered in the next post.
Facial dermatomes: ophthalmic nerve involvement can be serious