Status Cosmeticus: Are Your Efforts To Improve Your Complexion Making It Worse?
It’s good to have a nourishing skin care routine. But it is possible to do more harm than good when caring for the delicate skin of the face if you end up using too many skin care products or products that contain particular known irritants.
Have you ever heard the term “status asthmaticus”? Status asthmaticus is a condition in which a person with asthma becomes acutely reactive to almost every possible airborne allergen and it produces progressively worse (life-threatening) bronchitis. Status cosmeticus is sort of similar though it is NOT life-threatening. Some sources refer to this condition as Cosmetic Intolerance Syndrome (CIS) or the most extreme subset of Sensitive Skin Syndrome (SSS). It is a progressive irritation of the skin (most commonly of the delicate skin of the face) in which almost anything applied topically stings, burns, itches and/or causes inflammation. This acute reaction is not actually an allergic contact dermatitis (an immune response called Type IV Hypersensitivity Reaction), it is an irritant reaction. We know this because when patients with status cosmeticus undergo patch testing to determine the allergen causing the skin reaction, the tests are usually negative. In addition, “use tests” (applying the suspected substance to the antecubital fossa on the arm to see if the skin reacts) are likewise unremarkable. This reminds us that the skin of the face is definitely more sensitive than the rest of our skin and we have to be careful how we care for it. The good news is that status cosmeticus is most often temporary and it can be treated successfully with a little restrain and good lot of patience.
Many substances found in cosmetics and skin care products can cause negative skin reactions. In status cosmeticus, the patient is not reacting to any one particular ingredient, they are beginning to react to just about everything that they use on their face: soap, cleansers, makeup, moisturizers, shaving products, sunscreen, serums, and professional facial treatments (esp. chemical peels). It is as if the patient’s skin is so irritated that it simply can’t tolerate coming into prolonged contact with any more products. The typical person who develops status cosmeticus is someone who maintains a diligent skincare routine, someone who applies makeup to their face everyday, or someone who gets many facials or other professional skin treatments on their face. It is more common in women and in people with dry skin. Patients who already have rosacea, atopic dermatitis, seborrheic dermatitis, or perioral dermatitis are more likely to develop status cosmeticus.
In the beginning of this condition, the patient may not notice much in the way of symptoms. Perhaps their face stings a little when they sweat, especially on their cheeks or along the nasolabial folds (the smile lines leading from the corners of the mouth to the nostrils). As the skin’s sensitivity progresses, certain substances will cause stinging or burning when first applied to the face, though this discomfort usually subsides after a little while so the patient dismisses this as a symptom. Soon the burning or stinging becomes more pronounced or may linger longer after the initial application of cosmetics; between applications of any topical products the skin may feel tight and dry. The patient often will try tons of different products or brands of products because they “react to just about everything”. Eventually mild erythema (redness) will develop across the “butterfly” region of the face (across the cheeks and nose) and there may also be mild edema (swelling) of the eyelids. When status cosmeticus progresses to advanced stages, the skin becomes rough and dry with flakes or scales and the erythema (redness) can become permanent (similar to rosacea). If status cosmeticus is suspected and it does not respond to treatment (outlined below), further medical testing should be performed to rule out SLE (systemic lupus erythema, a serious autoimmune disease), rosacea, contact dermatitis or other inflammatory skin ailments.
TREATMENT OF STATUS COSMETICUS
When the skin is hyperreactive to most substances that come into contact with it, the most important thing to do is to minimize the number of skin care products applied until the inflammation and discomfort clears (in some severe cases it may even be necessary to avoid the use of all topical substances). This typically takes at least 6 weeks, up to several months, for symptoms to subside completely. For those patients who had previously adhered to a diligent skin care regiment, this make require a good amount of restraint. During the healing phase skin may feel tight and dry and even slightly itchy. Harsh commercially produced soaps and cleansers should be avoided. Gentle natural liquid or powder cleansers can be used, but should be used sparingly and never more than twice per day. Pat skin dry with a cotton towel (do not rub). Gentle natural carrier oils (such as olive oil, coconut oil, rosehip seed oil, jojoba oil, or some other less common oils) can be applied in very small amounts to help soften skin and hold in moisture. Rosewater or other flower hydrosols can be spritzed onto the face before application of the oil to better hydrate the skin. The use of any known irritating topical substances must be avoided (probably forever). Topical corticosteroids are not recommended for the treatment of status cosmeticus.
WHAT AGGRAVATES STATUS COSMETICUS?
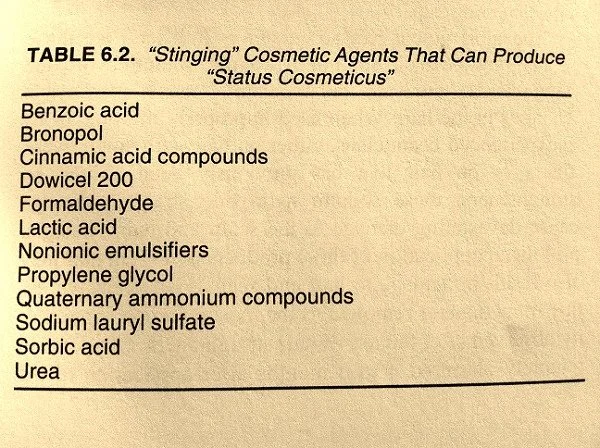
In addition to the specific list of known irritating ingredients (in the photo at right), anything that causes local trauma to the skin can exacerbate status cosmeticus. Dietary and environmental factors can also make the condition worse in many cases. Patients who think they have status cosmeticus should avoid the following:
These common skin care product ingredients can really irritate skin and should be avoided.
[courtesy Fisher’s Contact Dermatitis, 5th ed.]
General overuse of skin care products (even if they do not contain known irritants)
Over-exfoliation (overly frequent use of facial cleansing scrubs, skin brushes, exfoliating facial masks)
Sunburn
UV light therapy (used to treat other skin conditions or depression)
Cosmetic procedures such as dermabrasion, laser resurfacing, chemical peels
Facial surgeries, esp. facelifts
Very hot climates
Very cold climates
Dry climates
Hot water directly contacting the skin
Cold water directly contacting the skin
Extreme temperature changes (temperature of air or water contacting the skin)
Sun exposure
Wind
Pollution
Consumption of alcohol
Coffee
Spices/spicy foods
Hot beverages
Topical corticosteroids. Corticosteroid creams are often prescribed for patients who present to dermatologist offices complaining of facial rashes. But they have been reported to trigger status cosmeticus/Senstive Skin Syndrome (SSS) and prolonged use in the treatment of this condition should be avoided. In general, topical corticosteroids can thin the skin, making it more fragile. In the case of status cosmeticus/SSS, the skin already has decreased barrier function and the use of topical corticosteroids has led to tachyphylaxis (Tachyphylaxis is the tolerance the skin develops to the vasoconstrictive action of topical steroids. After repeated use of topical steroids, the capillaries in the skin do not constrict as well, requiring higher doses or more frequent application of the steroid.). This can lead to increasingly more severe erythema (redness and inflammation) that has the potential to become permanent. I would say this is especially risky in those with rosacea or atopic eczema.
Traditional Chinese Medicine (TCM) can be very helpful in healing status cosmeticus. Internal herbs are the treatment of choice and topical preparations can be helpful when prescribed properly. We shall cover these treatment options in the next post.
Sources used for this blog post:
Rietschel, Robert L. and Fowler, Joseph F, Jr. Fisher’s Contact Dermatology, 5e; 54- 55.
Lev-Tov H, Maibach HI. The Sensitive Skin Syndrome. Indian J Dermatol 2012;57:419-23
Pons-Guiraud A., Department of Dermatology, Hôpital Saint Louis, Paris, France. Sensitive skin: a complex and multifactorial syndrome. J Cosmet Dermatol. 2004 Jul;3(3):145-8.